Understanding the Pediatric Assessment Triangle
Pediatric emergencies present unique challenges because children often cannot describe what they feel, and their conditions can change quickly. In these high-stakes moments, healthcare providers must rely on both clinical experience and structured tools to guide decision-making. The Pediatric Assessment Triangle has become one of the most important rapid assessment methods for evaluating infants and children in urgent situations. Giving providers a clear framework for observation helps identify life-threatening conditions within seconds. This article explores what the Pediatric Assessment Triangle is, why it matters, and how it works alongside other assessment tools to improve pediatric care.
The Pediatric Assessment Triangle is a rapid, visual assessment method used to evaluate a child’s physiological status within the first few moments of contact. Its purpose is to help providers quickly determine whether a child is sick, and if so, how sick. Unlike traditional vital signs, which require equipment and time, the Triangle relies on observable signs that can be assessed immediately.

Why the PAT is Essential in Pediatric Emergency Care
Healthcare providers use it at the doorway of a room, at the scene of an emergency, or while approaching a patient in distress. The goal is to identify respiratory, circulatory, and neurological issues with speed and accuracy. Because children often compensate well until they suddenly decompensate, the PAT gives clinicians a fast way to recognize early warning signs before the situation becomes critical.
Providers rely heavily on the Pediatric Assessment Triangle because it bridges the gap between initial impression and more detailed assessments. It allows them to start forming a diagnosis even before touching the patient. When time is limited, being able to categorize a child as stable, unstable, or critically ill gives structure to urgent decision-making. It also helps communicate findings clearly during handoffs between emergency responders and hospital staff. The Triangle is not a replacement for a thorough examination, but it enhances efficiency by guiding priorities and highlighting areas that need immediate attention.
Understanding the Triangle Assessment of a Child
Understanding the Triangle requires breaking it down into its three components: Appearance, Work of Breathing, and Circulation to Skin. Appearance reflects neurological status and overall interaction with the environment. A child who is alert, active, and engaging typically has adequate brain perfusion and oxygenation. Providers look at muscle tone, facial expression, eye contact, and how the child interacts with caregivers. Work of Breathing emphasizes how much effort the child is using to breathe. Observing nasal flaring, retractions, abnormal breath sounds, or changes in posture helps identify respiratory distress early. Circulation to Skin focuses on the cardiovascular system. By assessing skin color, temperature, and signs of poor perfusion such as mottling or cyanosis, providers can quickly determine if the child is experiencing shock or inadequate blood flow. When these three elements are viewed together, patterns emerge that help identify whether the emergency is primarily respiratory, circulatory, or neurological.
What is the Mnemonic for the Pediatric Assessment Triangle?
Many clinicians use the TICLS mnemonic to help remember the key indicators of a child’s appearance. Tone refers to muscle strength and posture, which reflect neurological function. Interactiveness highlights how well the child responds to the environment and whether they show curiosity or engagement. Consolability examines how the child reacts to comfort from a caregiver, which can reveal subtle signs of distress. Look, or gaze, assesses eye contact, visual tracking, and whether the child appears focused or vacant. Speech or cry evaluates the strength, quality, and appropriateness of vocalizations based on age. When used together, TICLS provides a reliable method for judging appearance and allows providers to identify concerning changes quickly. Additional mnemonics may support breathing or circulation assessments, but TICLS remains one of the most widely taught tools for the Pediatric Assessment Triangle.
What Does ABC Mean in Pediatric Assessment Triangle?
The PAT also aligns closely with the ABC assessment, another foundational approach in emergency care. While the Triangle helps identify the general category of illness, the ABC method provides a structured approach for hands-on evaluation. Airway assessment begins by determining whether the child’s airway is open, obstructed, or at risk of compromise. Breathing assessment focuses on rate, rhythm, and the presence of abnormal effort or sounds. Circulation assessment includes pulse quality, capillary refill, and any signs of bleeding or shock. When providers combine PAT and ABC, they gain both a quick visual impression and a systematic method for immediate intervention. This integrated approach is essential in pediatric care, where seconds matter.
Clinical Applications and Case Examples
Clinical applications of the Pediatric Assessment Triangle span a wide range of emergencies. For example, distinguishing respiratory distress from respiratory failure can be lifesaving. A child with increased work of breathing but normal appearance and circulation may be compensating, whereas changes in appearance signal impending failure. Shock recognition becomes easier when poor circulation to the skin is paired with changes in breathing or mental status. Neurological emergencies often present with abnormal appearance, decreased tone, or altered interaction. In each case, the Triangle points providers toward the underlying problem before equipment-based assessments can be completed.
Common Pitfalls and Best Practices
Despite its effectiveness, providers can make mistakes when applying the Pediatric Assessment Triangle. Common pitfalls include focusing too much on a single component, overlooking subtle signs, or attempting to perform a full physical exam before forming an initial impression. Best practices involve observing the child from the moment they are seen, maintaining a calm approach, and reevaluating frequently as conditions change. Experience helps clinicians recognize variations in normal behavior across different ages, which further strengthens assessment accuracy.
Frequently Asked Questions
How long does it take to complete a Pediatric Assessment Triangle evaluation?
The PAT is designed to be completed in 30-60 seconds from the moment you first see the child. This rapid assessment doesn’t require any equipment or physical contact with the patient. Healthcare providers can perform the PAT from the doorway or across the room by simply observing the child’s appearance, breathing effort, and skin color. This quick evaluation allows for immediate identification of life-threatening conditions and helps prioritize treatment decisions without delay.
Can parents or non-medical professionals use the Pediatric Assessment Triangle?
While the PAT was developed for healthcare providers, parents and caregivers can benefit from understanding its basic principles. Recognizing when a child’s appearance is “off,” when they’re working hard to breathe, or when their skin color looks abnormal can help families identify when emergency care is needed. However, formal training in pediatric emergency assessment—such as that provided in PALS certification courses—is necessary to properly interpret findings and implement appropriate interventions based on PAT results.
What happens after the Pediatric Assessment Triangle identifies an abnormality?
When the PAT reveals an abnormality in one or more components, healthcare providers immediately move to hands-on assessment and intervention. The specific abnormality pattern guides treatment priorities—for example, abnormal work of breathing prompts focus on respiratory support, while abnormal circulation to skin triggers evaluation for shock. The PAT essentially acts as a visual “stop sign” that alerts providers to critical conditions requiring immediate attention, after which they follow established emergency protocols for pediatric resuscitation and stabilization.
Conclusion and Call to Action
The Pediatric Assessment Triangle represents a fundamental shift in how healthcare providers approach pediatric emergencies. By enabling rapid, accurate assessment without equipment or patient contact, the PAT saves precious seconds that can make the difference in a child’s outcome. Understanding this tool is essential for anyone who provides emergency care to children.
Whether you’re a healthcare professional looking to enhance your pediatric emergency skills or someone seeking to understand how medical teams evaluate sick children, proper training in pediatric life support is invaluable.
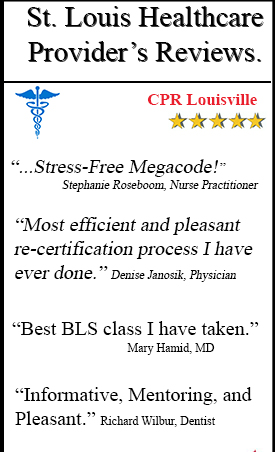
CPR Louisville, an American Heart Association training site, offers comprehensive PALS classes in Louisville that cover the Pediatric Assessment Triangle and other critical pediatric emergency protocols. Our stress-free, hands-on courses provide the practical experience you need to confidently assess and treat pediatric patients in crisis situations.
We also offer initial certifications and renewals in BLS for Healthcare Providers, ACLS, and CPR and First Aid courses—all designed to give you the skills and confidence to respond effectively in emergencies. Don’t wait until you’re faced with a pediatric emergency to wish you had better training.
Contact CPR Louisville today to enroll in our PALS classes in Louisville and gain the expertise to make a life-saving difference for children in your care.