In the realm of emergency medical care, two acronyms stand out as pillars of life-saving interventions: BLS (Basic Life Support) and ACLS (Advanced Cardiovascular Life Support). BLS encompasses fundamental techniques aimed at sustaining life during emergencies, while ACLS builds upon these basics to address more complex cardiac events. Understanding the symbiotic relationship between BLS and ACLS is paramount for healthcare professionals tasked with delivering effective emergency care.
Fundamentals of BLS
At the core of BLS lies the objective of preserving life through swift and decisive actions. This involves mastering key components such as chest compressions, rescue breaths, and the use of automated external defibrillators (AEDs). The significance of early recognition and intervention cannot be overstated, particularly in cardiac arrest scenarios where every second counts.
Chest Compressions: Compressions are the cornerstone of BLS, aimed at maintaining blood circulation to vital organs until more advanced interventions can be administered. Proper technique, including adequate depth and rate, is essential for maximizing the effectiveness of compressions.
Rescue Breaths: Rescue breaths complement chest compressions by providing oxygen to the patient’s lungs and bloodstream. The ratio of compressions to breaths, typically 30:2 for single-rescuer CPR, ensures a balance between oxygenation and circulation.
AED: The utilization of AEDs has revolutionized cardiac arrest management by enabling early defibrillation in the community setting. These portable devices analyze the heart’s rhythm and deliver a shock if indicated, potentially restoring normal cardiac function.
Early recognition of cardiac arrest and prompt initiation of BLS interventions significantly improve patient outcomes, underscoring the importance of widespread BLS training and public access to AEDs.
Advancing to ACLS
ACLS represents the next level of care, integrating advanced techniques and interventions to address critical cardiac events. Building upon the foundation laid by BLS, ACLS introduces concepts such as advanced airway management, intravenous access, medication administration, and ECG interpretation. This transition marks a crucial shift from basic to advanced life support measures, requiring healthcare providers to possess a deeper understanding of cardiac physiology and emergency management.
Advanced airway management techniques, including endotracheal intubation and supraglottic airway devices, are employed to secure the patient’s airway and facilitate effective ventilation. Proper airway management is essential for ensuring adequate oxygenation and ventilation, particularly in patients with compromised respiratory function.
Intravenous access allows for the administration of medications and fluids directly into the bloodstream, enabling rapid delivery of life-saving interventions. ACLS algorithms outline specific medication protocols based on the patient’s underlying cardiac rhythm and clinical presentation, emphasizing the importance of accurate dosing and timing.
ECG interpretation plays a pivotal role in ACLS, guiding treatment decisions and identifying arrhythmias that require immediate intervention. Healthcare providers must be proficient in recognizing various ECG patterns, including ventricular fibrillation, ventricular tachycardia, atrial fibrillation, and asystole, to effectively manage cardiac emergencies.
The integration of advanced ACLS interventions with BLS techniques ensures a comprehensive approach to resuscitation, optimizing patient outcomes and survival rates. Healthcare providers must undergo regular ACLS training and certification to maintain proficiency in these advanced life support skills.
Understanding the Relationship Between BLS and ACLS
BLS serves as the foundation upon which ACLS interventions are built. The seamless integration of BLS techniques within ACLS protocols ensures a continuum of care from the initial recognition of an emergency to the implementation of advanced interventions. Effective BLS not only primes patients for successful ACLS interventions but also improves overall outcomes by optimizing the patient’s physiological state before the initiation of advanced measures.
The transition from BLS to ACLS represents a critical progression in the resuscitation process, highlighting the importance of early recognition and intervention in determining patient outcomes. By recognizing the signs of deterioration and initiating BLS measures promptly, healthcare providers can facilitate a smooth transition to ACLS interventions, minimizing the time to definitive treatment.
Studies have demonstrated the significant impact of high-quality BLS on patient survival rates, underscoring the pivotal role of basic interventions in the chain of survival. By emphasizing the importance of early CPR and defibrillation, healthcare systems can improve outcomes for patients experiencing cardiac arrest in both out-of-hospital and in-hospital settings.
The relationship between BLS and ACLS extends beyond the clinical realm to include education and training. Healthcare providers must possess a solid foundation in BLS principles before advancing to ACLS certification, ensuring competency in basic resuscitation techniques before mastering more advanced interventions.
Case Studies and Real-Life Examples
Examining real-life scenarios provides insights into the intrinsic relationship between BLS and ACLS. Success stories underscore the critical role of BLS in initiating ACLS interventions, demonstrating how timely and effective basic interventions pave the way for advanced care. Furthermore, teamwork between BLS and ACLS providers has been shown to significantly enhance patient survival rates, emphasizing the importance of seamless coordination in emergency situations.
Consider a case where a bystander witnesses a sudden collapse and immediately initiates CPR. By promptly activating emergency medical services (EMS) and retrieving an AED, the bystander ensures timely defibrillation upon its arrival. EMS providers continue resuscitative efforts upon their arrival, seamlessly transitioning from BLS to ACLS interventions as needed. The patient is successfully resuscitated and transported to the hospital for further care, highlighting the critical role of integrated BLS and ACLS protocols in achieving positive outcomes.
In another scenario, a healthcare provider identifies a patient in cardiac arrest within a hospital setting and initiates ACLS interventions without delay. However, due to delays in BLS interventions, the patient’s chances of survival are compromised, emphasizing the importance of early recognition and intervention in optimizing outcomes. Through ongoing training and quality improvement initiatives, healthcare systems can address gaps in the delivery of BLS and ACLS interventions, ultimately improving patient care and outcomes.
Training and Certification
Comprehensive training in both BLS and ACLS is essential for healthcare professionals entrusted with emergency care responsibilities. Certification requirements typically encompass rigorous coursework, hands-on practice sessions, and assessments to ensure proficiency in life-saving techniques. Various resources and training avenues exist to accommodate different learning styles and preferences, ranging from traditional classroom settings to online courses and simulation-based training programs.
BLS training emphasizes the importance of early recognition, activation of the emergency response system, and high-quality CPR techniques. Participants learn to assess the scene for safety, check for responsiveness, and initiate chest compressions and rescue breaths as needed. A thorough understanding of AED operation and basic airway management techniques is also essential for BLS certification.
ACLS certification builds upon the foundation of BLS, providing healthcare providers with the knowledge and skills to manage cardiac emergencies in both adult and pediatric patients. Participants learn to identify and treat various arrhythmias, administer appropriate medications, and coordinate resuscitation efforts as part of a multidisciplinary team. ACLS training incorporates simulation-based scenarios to enhance clinical decision-making and teamwork skills, preparing providers to effectively manage complex cardiac events in real-world settings.
Challenges and Future Directions
Despite the advancements in resuscitation science, challenges persist in implementing effective BLS and ACLS protocols. Issues such as resource constraints, disparities in access to training, and variability in practice standards pose ongoing challenges for healthcare systems worldwide. However, emerging trends and advancements in technology offer promising avenues for improving resuscitation outcomes. Strategies aimed at enhancing the synergy between BLS and ACLS, such as integrated training approaches and standardized protocols, hold the potential to further optimize emergency care delivery.
One of the challenges in resuscitation training is ensuring consistent adherence to evidence-based guidelines and best practices across healthcare settings. Variability in training quality and retention rates among healthcare providers can impact the delivery of BLS and ACLS interventions, highlighting the need for ongoing education and quality improvement initiatives. Standardized training curricula, regular skills assessments, and performance feedback mechanisms can help standardize resuscitation practices and ensure competency among healthcare providers.
Another challenge is the integration of new technologies and techniques into resuscitation training and practice. While advancements such as high-fidelity simulation and virtual reality offer immersive learning experiences, their implementation may require significant investments in infrastructure and training resources. Healthcare systems must carefully evaluate the cost-effectiveness and feasibility of adopting new technologies to enhance resuscitation training and improve patient outcomes.
In addition to addressing technical challenges, healthcare systems must also consider the psychological and emotional impact of participating in resuscitation efforts. Healthcare providers involved in cardiac arrest resuscitations may experience stress, anxiety, and emotional distress, particularly in high-pressure environments such as the emergency department or intensive care unit. Supportive resources and debriefing sessions can help providers cope with the emotional toll of resuscitation efforts and prevent burnout.
Science holds promise for continued advancements in patient care and outcomes. Research efforts aimed at refining resuscitation techniques, optimizing post-resuscitation care, and identifying novel therapeutic targets are underway, offering hope for further improvements in survival rates and neurological outcomes following cardiac arrest. By embracing innovation and collaboration, healthcare systems can overcome current challenges and pave the way for a future where every patient has the best possible chance of survival and recovery.
The connection between BLS and ACLS forms the cornerstone of effective emergency medical care. Healthcare professionals must recognize the indispensable role of BLS in laying the groundwork for successful ACLS interventions. By prioritizing proficiency in both BLS and ACLS, providers can significantly impact patient outcomes and contribute to saving lives. As we continue to evolve in our understanding and practice of resuscitation medicine, mastering these life-saving skills remains paramount in ensuring the best possible outcomes for patients in critical situations. Through ongoing education, training, and quality improvement initiatives, healthcare systems can enhance the synergy between BLS and ACLS, ultimately improving patient care and survival rates in cardiac emergencies.
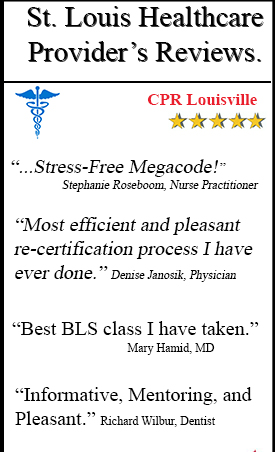
In conclusion, grasping the interdependence between Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS) is pivotal for healthcare professionals. The seamless coordination between these two skill sets can significantly enhance patient outcomes in emergency situations. As highlighted by CPR Louisville, obtaining certifications in ACLS and BLS through reputable training sites such as theirs, which also cater to ACLS certification in Louisville and BLS certification in Louisville, ensures that medical practitioners are equipped with the latest knowledge and techniques. By prioritizing comprehensive training and continuous education, healthcare providers can confidently respond to critical situations, ultimately saving lives and promoting a healthier community.