In the critical moments following cardiac arrest or respiratory failure, the method of ventilation can significantly impact patient outcomes. The comparison between mouth-to-mouth resuscitation and bag-mask ventilation represents one of the most important discussions in emergency medical care. This article examines the evidence-based differences between these two approaches, evaluating their effectiveness, practical considerations, and the situations where one method may be preferable to the other.
The Evolution of Resuscitation Techniques
The history of resuscitation spans centuries, with mouth-to-mouth ventilation documented as early as biblical times. However, modern emergency medicine has introduced alternative methods, including bag-mask ventilation, which has become standard equipment for healthcare providers. Understanding how these techniques have evolved provides valuable context for evaluating their effectiveness in contemporary emergency care scenarios.
Mouth-to-mouth ventilation, a cornerstone of traditional CPR, involves the direct transfer of exhaled air from the rescuer to the patient. In contrast, bag-mask ventilation utilizes a manual resuscitator consisting of a self-inflating bag, a one-way valve system, and a face mask to deliver oxygen-enriched air to the patient. Both techniques aim to provide artificial ventilation, but they differ significantly in their application, efficacy, and acceptability in various emergency scenarios.
Mouth-to-Mouth vs. Bag-Mask: Technical Considerations
When comparing mouth-to-mouth and bag-mask ventilation, several technical factors warrant consideration. These elements directly influence the quality of ventilation provided and, consequently, the patient’s chances of survival.
Oxygen Delivery Efficiency
Mouth-to-mouth ventilation delivers approximately 16-17% oxygen concentration, reflecting the oxygen content of exhaled air. In contrast, bag-mask devices connected to supplemental oxygen can provide nearly 100% oxygen concentration, representing a substantial advantage in oxygen delivery. This difference becomes particularly significant during prolonged resuscitation efforts, where higher oxygen concentrations may help prevent hypoxic damage to vital organs.
Research demonstrates that the higher oxygen concentrations achievable with bag-mask systems can lead to improved blood oxygenation levels. A study published in the Journal of Emergency Medicine found that patients receiving bag-mask ventilation with supplemental oxygen maintained higher arterial oxygen levels compared to those receiving mouth-to-mouth ventilation.
Tidal Volume Control
Delivering appropriate tidal volumes—the amount of air moved into and out of the lungs during normal breathing—represents another critical difference between these techniques. Mouth-to-mouth ventilation often results in variable tidal volumes, depending on the rescuer’s lung capacity and technique. Conversely, bag-mask devices allow for more consistent tidal volume delivery through standardized bag sizes and pressure-relief valves.
Excessive tidal volumes can cause gastric inflation, increasing the risk of regurgitation and aspiration. Studies indicate that both methods can result in excessive volumes when performed by inexperienced rescuers. However, bag-mask devices offer better control mechanisms to mitigate this risk when used properly.
Airway Management Challenges
Both ventilation methods present unique challenges in managing the airway effectively. Mouth-to-mouth technique requires establishing a proper seal between the rescuer’s mouth and the patient’s mouth, which can be difficult to maintain, particularly during prolonged resuscitation. Bag-mask ventilation demands proper mask positioning and sealing against the face, along with coordinated bag compression.
Research consistently shows that maintaining an effective mask seal represents one of the most challenging aspects of bag-mask ventilation, especially for single rescuers. A study in Resuscitation found that two-rescuer bag-mask ventilation significantly improved tidal volume delivery and reduced leakage compared to the single-rescuer technique.
Clinical Outcomes: What the Research Shows
The ultimate measure of any resuscitation technique lies in its ability to improve survival rates and neurological outcomes. Examining the evidence comparing mouth-to-mouth and bag-mask ventilation reveals important insights for emergency care protocols.
Survival Rates
Multiple studies have compared survival-to-discharge rates between patients receiving mouth-to-mouth versus bag-mask ventilation. A meta-analysis published in Circulation found no statistically significant difference in survival rates between the two methods when performed by trained healthcare providers. However, when stratified by rescuer experience, bag-mask ventilation showed slightly better outcomes when performed by highly trained professionals.
Interestingly, compression-only CPR (without ventilation) has gained support for lay rescuers in adult sudden cardiac arrest, with some studies showing comparable or even better outcomes compared to traditional CPR with mouth-to-mouth ventilation. This finding has influenced recent guideline changes that prioritize chest compressions for lay rescuers.
Neurological Outcomes
Beyond survival, neurological function represents a crucial outcome measure. A prospective cohort study published in Resuscitation examined neurological outcomes using the Cerebral Performance Category scale. The study found that patients receiving bag-mask ventilation with supplemental oxygen demonstrated marginally better neurological outcomes at hospital discharge compared to those receiving mouth-to-mouth ventilation.
These findings suggest that the higher oxygen concentrations achievable with bag-mask ventilation may contribute to better cerebral oxygenation during cardiac arrest, potentially preserving neurological function. However, more research is needed to definitively establish this relationship.
Mouth-to-Mouth vs. Bag-Mask: Practical Considerations
Beyond clinical efficacy, practical considerations significantly influence the choice between mouth-to-mouth and bag-mask ventilation in real-world emergencies.
Disease Transmission Concerns
One of the most significant barriers to performing mouth-to-mouth ventilation is the fear of disease transmission. Despite the relatively low documented risk of infection transmission during mouth-to-mouth resuscitation, perception of risk remains high among both healthcare providers and lay rescuers.
Bag-mask devices eliminate direct contact between the rescuer and the patient’s airways, substantially reducing disease transmission concerns. This advantage has become increasingly relevant during infectious disease outbreaks, including the COVID-19 pandemic, where respiratory droplet transmission represents a primary concern.
Skill Acquisition and Retention
The learning curve for each technique differs substantially. Mouth-to-mouth ventilation requires minimal equipment knowledge but demands proper technique to establish an effective seal and deliver appropriate volumes. Bag-mask ventilation requires familiarity with equipment assembly and operation, but offers standardized delivery once mastered.
Studies examining skill retention show that bag-mask ventilation skills deteriorate more rapidly than mouth-to-mouth skills without regular practice. A simulation study found that healthcare providers demonstrated a significant decline in bag-mask proficiency after six months without practice, while mouth-to-mouth skills showed better retention.
Rescuer Fatigue
During prolonged resuscitation efforts, rescuer fatigue becomes an important consideration. Mouth-to-mouth ventilation requires the rescuer to repeatedly deliver forceful exhalations, which can be exhausting. Bag-mask ventilation demands hand strength and coordination but may be less physically taxing over extended periods.
A comparative study measuring rescuer exertion found that mouth-to-mouth ventilation resulted in higher perceived effort and greater decrease in performance quality over time compared to bag-mask ventilation during prolonged resuscitation scenarios.
Special Populations: Pediatric Considerations
The comparison between mouth-to-mouth and bag-mask ventilation takes on additional dimensions when considering pediatric emergencies, where respiratory causes of arrest predominate over cardiac causes.
Anatomical Differences
Children’s airways differ significantly from adults, with larger tongues relative to oral cavity size, softer tracheal cartilage, and narrower airways. These differences make proper technique especially crucial for both ventilation methods. However, they can also make establishing an effective seal with a mask more challenging in pediatric patients.
Research in pediatric resuscitation indicates that mouth-to-mouth ventilation may provide more reliable tidal volumes in infants and young children when performed by providers with limited experience. Conversely, pediatric bag-mask devices with appropriately sized masks perform exceptionally well in the hands of experienced providers.
Rescue Breathing Importance
While compression-only CPR has gained acceptance for adult cardiac arrest, ventilation remains essential in pediatric resuscitation due to the primarily respiratory nature of most pediatric arrests. Both the American Heart Association and European Resuscitation Council emphasize the continued importance of rescue breathing in pediatric resuscitation protocols, regardless of whether mouth-to-mouth or bag-mask techniques are employed.
Training Implications: Developing Effective Skills
The effectiveness of both mouth-to-mouth and bag-mask ventilation depends significantly on proper training and skill maintenance. Understanding the training requirements for each method helps inform decisions about educational programs and certification standards.
Simulation-Based Training
Simulation training has proven particularly effective for developing proficiency in both ventilation techniques. High-fidelity mannequins that help provide feedback on ventilation volume and effectiveness, learners develop proper technique. Studies show that training programs incorporating such feedback significantly improve performance for both methods.
For bag-mask ventilation specifically, studies demonstrate that targeted training focusing on proper hand positioning, mask seal techniques, and coordinated bag compression improves performance. Similarly, mouth-to-mouth ventilation benefits from specific instruction on head positioning, airway opening, and effective seal formation.
Refresher Training Frequency
Research on skill retention suggests that both ventilation methods benefit from regular refresher training. However, bag-mask ventilation skills appear to require more frequent practice to maintain proficiency. A study published in Resuscitation recommended refresher training every 3-6 months for bag-mask techniques, while mouth-to-mouth skills showed acceptable retention for up to 12 months.
These findings have important implications for certification programs and continuing education requirements for healthcare providers and first responders who must maintain competence in these critical skills.
Guidelines and Recommendations: Current Standards
Professional organizations regularly update guidelines for resuscitation based on emerging evidence. Current recommendations regarding mouth-to-mouth versus bag-mask ventilation reflect a nuanced approach based on rescuer training, available equipment, and scenario specifics.
Healthcare Provider Recommendations
For healthcare providers with proper training, bag-mask ventilation with supplemental oxygen represents the preferred method in most situations. The American Heart Association’s Basic Life Support guidelines recommend bag-mask ventilation as the primary method for healthcare providers, citing the advantages of higher oxygen delivery and reduced disease transmission risk.
However, these guidelines also acknowledge that mouth-to-mouth ventilation remains an acceptable alternative when equipment is unavailable or in situations where establishing an effective mask seal proves exceptionally difficult.
Lay Rescuer Considerations
For lay rescuers, current guidelines offer flexibility. While compression-only CPR has become the recommended approach for untrained rescuers witnessing adult sudden cardiac arrest, traditional CPR, including mouth-to-mouth ventilation, remains in the guidelines for those willing and trained to provide it.
The emphasis has shifted toward ensuring high-quality chest compressions without interruption, recognizing that the benefits of continuous compressions may outweigh the advantages of ventilation in the early minutes of adult cardiac arrest for lay rescuers.
Making the Right Choice: Context Matters
The comparison between mouth-to-mouth and bag-mask ventilation ultimately depends on multiple contextual factors. Understanding these considerations helps emergency responders make appropriate decisions in diverse scenarios.
Available Resources
Resource availability often dictates ventilation method choice. In hospital settings with ready access to bag-mask devices and supplemental oxygen, bag-mask ventilation represents the logical choice. In remote or resource-limited settings where specialized equipment may be unavailable, mouth-to-mouth ventilation provides a viable alternative requiring no equipment beyond a simple face shield.
Rescuer Expertise
Rescuer training and experience significantly influence which method will provide better outcomes. Studies consistently show that highly trained providers achieve superior results with bag-mask ventilation, while those with minimal training may provide more effective ventilation using mouth-to-mouth techniques. This finding underscores the importance of matching the method to the rescuer’s skill level.
Situation Specifics
The specific emergency scenario may favor one method over the other. For example, in suspected opioid overdose cases where providing supplemental oxygen is particularly beneficial, bag-mask ventilation with oxygen represents the preferred approach when available. Conversely, in drowning incidents where immediate ventilation is critical and equipment may not be readily accessible, mouth-to-mouth ventilation enables rapid intervention.
Conclusion: A Balanced Approach
The comparison between mouth-to-mouth and bag-mask ventilation reveals that both methods maintain important roles in emergency care. Rather than viewing them as competing techniques, a more productive approach recognizes their complementary nature within a comprehensive emergency response system.
Healthcare institutions and training programs should ensure providers develop competence in both methods, understanding the advantages, limitations, and appropriate applications of each. This balanced approach maximizes flexibility in emergency response and optimizes patient outcomes across diverse scenarios.
The evidence suggests that when performed correctly by trained providers, both methods can support effective resuscitation. The choice between mouth-to-mouth and bag-mask ventilation should be guided by rescuer training, available resources, and specific emergency circumstances rather than rigid adherence to a single approach.
Get Certified Today: Life-Saving Skills Within Reach
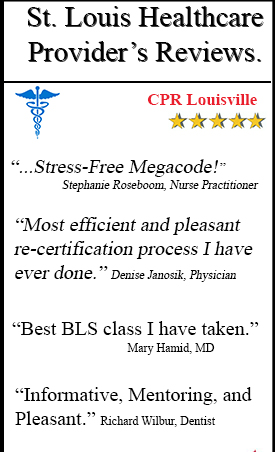
Developing proficiency in both mouth-to-mouth and bag-mask ventilation techniques requires proper training under expert guidance. CPR Cincinnati offers comprehensive American Heart Association certification courses that provide hands-on experience with both ventilation methods.
Whether you’re seeking CPR certification or BLS certification in Louisville, our stress-free, interactive courses equip you with the knowledge and skills to respond effectively in emergencies. As an American Heart Association training site, we offer initial certifications and renewals in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses.
Don’t wait until an emergency occurs to prepare yourself. Contact CPR Louisville today to enroll in the best CPR training in Cincinnati and gain the confidence to save lives when it matters most.