The Critical Importance of Airway Management in ACLS
In the world of emergency medicine, airway management is often the first and most vital step in saving a life during cardiac arrest. In Advanced Cardiac Life Support (ACLS) scenarios, establishing and maintaining a patent airway is the bedrock upon which all other resuscitation efforts depend. Data consistently shows that patients who receive timely and effective airway interventions have significantly higher survival rates. Without a clear and secure airway, even perfect chest compressions or early defibrillation won’t ensure oxygen delivery to vital organs, making skilled airway management a non-negotiable component of successful resuscitation.
Overview of ACLS Airway Hierarchy
ACLS airway techniques follow a progressive hierarchy—from basic non-invasive methods to advanced, definitive procedures. Healthcare providers must understand when and how to escalate airway interventions based on the patient’s condition, the effectiveness of current techniques, and the resources available. Each level of airway support has its considerations, advantages, and potential complications.
What Healthcare Providers Will Learn
This article will walk you through the core techniques used in ACLS airway management—from the bag-valve-mask (BVM) to supraglottic airways (SGAs) and endotracheal intubation—highlighting evidence-based practices, common pitfalls, and best strategies for success. Whether you’re a new provider or a seasoned clinician, understanding and mastering these techniques can profoundly impact patient survival and outcomes.
Bag-Valve-Mask (BVM) Ventilation: The Foundation
Bag-valve-mask ventilation is the foundation of emergency airway support. It’s often the first technique used when a patient is not breathing adequately or at all.
Proper BVM Technique
The BVM system is a non-invasive tool that delivers positive-pressure ventilation and can be used in virtually any setting. The most effective method is the two-person technique. One provider uses both hands to secure the mask on the patient’s face, creating a proper seal, while the other squeezes the bag to deliver breaths. This approach helps minimize air leaks and ensures consistent chest rise with each breath. Ideally, providers should deliver one breath every 5 to 6 seconds (10 to 12 breaths per minute), using just enough volume to see the chest rise, avoiding overinflation.
Common BVM Mistakes and Solutions
Despite being simple in theory, BVM use is often performed poorly in practice. Common mistakes include an inadequate mask seal, which leads to insufficient ventilation, and hyperventilation, which can increase intrathoracic pressure and reduce cardiac output. Additionally, delivering too much volume or pressure can cause air to enter the stomach—a phenomenon known as gastric insufflation, which can result in vomiting and aspiration. To optimize performance, providers should ensure proper head positioning with a head-tilt chin-lift or jaw-thrust maneuver and verify that the mask fits the patient’s facial structure. Equipment selection also matters.
BVM Selection and Equipment Considerations
Adult and pediatric patients require different BVM sizes and oxygen flow rates. Providers must assess whether BVM is sufficient or if they need to escalate to more advanced airway techniques.
Supraglottic Airways: The Intermediate Solution
When BVM ventilation is inadequate or unsustainable, supraglottic airways offer a valuable next step. These devices serve as intermediate solutions between basic BVM and endotracheal intubation.
Laryngeal Mask Airway (LMA) Insertion
The Laryngeal Mask Airway (LMA) is one of the most widely used SGAs. It’s easy to insert, requires minimal training, and provides a more stable airway than a mask alone.
King Laryngeal Tube (LT) Application
Another popular device, particularly in the pre-hospital setting, is the King Laryngeal Tube (LT). It’s designed for blind insertion and seals both the esophagus and pharynx to direct airflow into the trachea.
When to Choose Supraglottic Airways
SGAs are especially useful in situations where intubation is delayed, difficult, or outside the scope of the provider. While not a replacement for definitive airway control, they serve as effective temporary solutions and are commonly used during cardiac arrest resuscitation.
Endotracheal Intubation: The Gold Standard
The gold standard for airway management remains endotracheal intubation. This technique involves inserting a tube directly into the trachea to establish a protected and controlled airway. Intubation allows for precise ventilation and significantly reduces the risk of aspiration. However, it requires a high level of skill and preparation.
Pre-Intubation Assessment and Preparation
Before attempting intubation, providers must conduct a pre-intubation assessment, checking for potential complications and gathering all necessary equipment, such as laryngoscope blades, endotracheal tubes, a stylet, and a capnography device.
Direct Laryngoscopy Technique
Traditionally, direct laryngoscopy is used to visualize the vocal cords, but video laryngoscopy has become increasingly common.
Video Laryngoscopy Advantages
Video laryngoscopes offer a magnified, illuminated view of the airway on a screen, improving first-pass success rates, especially in patients with difficult airways.
Intubation Confirmation Methods
After intubation, verifying proper tube placement is critical. Continuous waveform capnography is the most reliable confirmation method. It provides real-time feedback on exhaled carbon dioxide, ensuring that the tube is in the trachea. Other confirmation techniques include auscultation, chest rise observation, and esophageal detector devices, but none are as definitive as capnography.
Alternative Airway Techniques
In rare, extreme situations when all other methods fail, cricothyrotomy may be required. This surgical airway technique is reserved for “can’t intubate, can’t ventilate” emergencies.
Cricothyrotomy: The Last Resort
It involves creating an incision through the cricothyroid membrane to access the trachea. While rarely performed, every provider should be familiar with the procedure in case it’s needed.
Nasopharyngeal and Oropharyngeal Airways
Additionally, airway adjuncts like nasopharyngeal (NPA) and oropharyngeal (OPA) airways are frequently used in earlier stages to maintain patency. NPAs are well tolerated by semi-conscious patients, while OPAs are reserved for those who are fully unconscious to avoid triggering a gag reflex. These simple tools are invaluable in facilitating BVM ventilation, especially during the initial response.
Airway Management During Special Circumstances
Cardiac Arrest Airway Priorities
Airway management during ACLS must also be adapted to special situations. In cardiac arrest, the immediate priority is high-quality chest compressions and defibrillation, with airway support tailored to avoid interruptions.
Respiratory Arrest Management
In respiratory arrest without cardiac compromise, securing the airway becomes the central focus.
Pediatric Airway Considerations
Pediatric airways add another layer of complexity due to anatomical differences. Providers must choose age-appropriate equipment and adjust techniques accordingly, especially when it comes to BVM ventilation and intubation.
Team Communication and Airway Management
Effective Team Dynamics
Effective airway management hinges not only on clinical skill but also on teamwork and communication. In a code situation, roles must be assigned, and providers must communicate with precision. The team leader ensures that one member is focused solely on the airway, while others manage compressions, defibrillation, and medication administration.
Quality Improvement in Airway Management
Post-resuscitation debriefings and quality improvement reviews help identify what went well and what can be improved. This feedback loop is essential for improving outcomes and refining skills.
Staying Current with Best Practices
Maintaining airway management competency requires consistent training. Skills like intubation can decay without regular practice. Simulation labs, ACLS refresher courses, and peer-reviewed learning opportunities are essential for staying sharp. Guidelines and technology continue to evolve, and providers must stay informed to ensure they’re using the most effective, up-to-date practices.
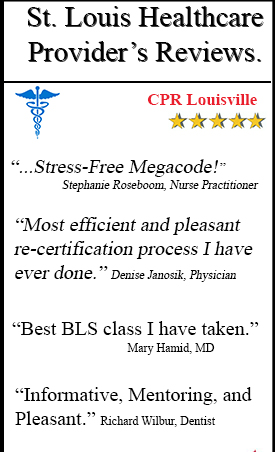
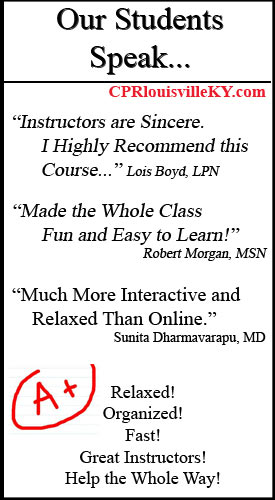
Don’t wait for an emergency to discover gaps in your airway management skills. Enroll in CPR Louisville’s comprehensive ACLS certification course today. Our hands-on, stress-free training environment ensures you’ll gain the confidence and competence needed to save lives. Contact us now to secure your spot in our next class.