Understanding CPR with an Advanced Airway: An Overview
When a person collapses from sudden cardiac arrest, the outcome hinges on two things: time and the quality of intervention. Proper airway management is one of the most vital components that dramatically improve CPR outcomes, transforming a desperate situation into one with a genuine chance of survival. In the high-stakes environment of resuscitation, a major change occurs in the Cardiopulmonary Resuscitation technique once a dedicated breathing tube, known as an advanced airway, is secured. An advanced airway in resuscitation refers to sophisticated devices like an endotracheal tube or ETT, or various supraglottic airways, such as the laryngeal mask airway, which create a sealed conduit directly into the patient’s trachea or pharynx. This secured connection fundamentally alters the traditional rhythm of CPR, introducing the concept of continuous chest compressions and asynchronous ventilations. Understanding this critical shift—the differences in compression and ventilation rates, the current guidelines from the American Heart Association, or AHA, and the required training—is essential for every provider involved in ACLS airway management.

What is an Advanced Airway in CPR?
Before detailing how CPR is performed differently when an advanced airway is in place, it is helpful to establish what constitutes an advanced airway and why it is so crucial in cardiac arrest management. An advanced airway device is placed by trained personnel to isolate the airway. This isolation prevents stomach contents from entering the lungs, a significant risk during standard CPR, and ensures that every breath delivered goes directly to the pulmonary system. In the context of Advanced Cardiovascular Life Support, securing the airway is a primary intervention because it allows for superior control over oxygenation and ventilation, creating an environment where life-saving drugs and defibrillation can be more effective. The presence of this secure, sealed pathway is the direct cause of the change in the CPR technique compared to the standard, basic life support approach. These devices, whether an endotracheal tube or one of the supraglottic options, represent a significant clinical advantage.
Standard CPR Without an Advanced Airway
To appreciate the efficiency gained with advanced airway CPR, one must first remember the standard protocol without it. Standard CPR without an advanced airway is characterized by the need to interrupt chest compressions to deliver breaths. In adult resuscitation, the standard ratio of compression-to-ventilation is thirty compressions followed by two ventilations, meaning the team must pause the critical work of circulating blood to give two breaths. While these pauses are necessary to oxygenate the patient when only a bag-mask device is used, they inherently lead to significant challenges. Each interruption, even for a few seconds, causes a detrimental drop in coronary and cerebral perfusion pressure, directly reducing the chances of a positive outcome. The AHA guidelines emphasize the profound negative impact of these interruptions, making the ability to minimize them a main goal of ACLS airway management.
How CPR Changes with an Advanced Airway in Place
The methodology of how CPR changes with an advanced airway in place marks a radical and necessary departure from the standard 30:2 ratio. The main difference is straightforward: there is no longer a need to pause chest compressions for ventilations. Instead, the team can focus on continuous chest compressions, aiming for a rate of 100 to 120 compressions every minute. The ventilation strategy shifts to asynchronous ventilations, meaning the breaths are delivered independently of the compression cycle. The new ventilation rate is one breath every six seconds, equating to approximately ten ventilations per minute. During this continuous process, the team must prioritize monitoring the patient’s physical chest rise to confirm the effectiveness of the ventilation, rather than pausing the compressions. Furthermore, for the highest quality resuscitation, providers should utilize waveform capnography, a non-invasive monitoring tool, not only to confirm the proper placement of the endotracheal tube but also to provide real-time feedback on the effectiveness of the chest compressions, ensuring optimal circulation is maintained.
Benefits of Advanced Airway CPR
The adoption of continuous chest compressions and asynchronous ventilations offers tangible benefits that translate directly to improved patient survival. The most significant advantage is the minimization of interruptions to chest compressions, leading to much better perfusion of the heart and brain. This constant circulation is the key factor linking advanced airway CPR to improved patient survival. Beyond continuity, an advanced airway allows for better oxygenation and overall ventilation management because the sealed circuit is more efficient and reliable than a standard mask. Logistically, this allows the resuscitation team to operate more smoothly, as team members can work simultaneously, with one dedicated compressor and one dedicated ventilator, maximizing efficiency during the arrest. These benefits are strongly supported by clinical evidence, leading to key updates in the AHA guidelines, which continue to advocate for this approach when an advanced airway is placed.
Potential Risks and Considerations
While the benefits are clear, utilizing an advanced airway also introduces potential risks and important considerations that require a high level of expertise. The primary risk is the simple but catastrophic error of incorrect placement, which can completely compromise oxygen delivery and ventilation, turning an intended life-saving measure into a lethal one. Another critical consideration is the danger of over-ventilation—delivering breaths too quickly or with too much force. This practice can lead to gastric insufflation, pushing air into the stomach, but more dangerously, it increases intrathoracic pressure. An elevated pressure inside the chest cavity reduces the venous return of blood to the heart, effectively canceling out the benefit of the continuous compressions. For these reasons, mastering the placement, securing, and appropriate ventilation rate for advanced airway CPR necessitates the exclusive involvement of highly trained providers; this is an intervention that is simply not appropriate for lay rescuers.
Real-Life Application: CPR in Hospitals vs. Prehospital Settings
The principles of advanced airway CPR are applied differently across various real-life clinical settings. In the hospital, staff in the emergency room, intensive care unit, and those with ACLS airway management certification are constantly prepared to implement these techniques. Conversely, in the prehospital setting, paramedics and emergency medical services personnel frequently manage cardiac arrest in uncontrolled environments, making the successful placement of an endotracheal tube a challenging but essential part of their practice. For instance, the dynamics of a street-side resuscitation differ significantly from those within a controlled operating theater, but the underlying guideline remains consistent: once an advanced airway is placed, the compression-to-ventilation ratio switches to continuous compressions and asynchronous breathing to maximize perfusion.
The Role of Training and Certification
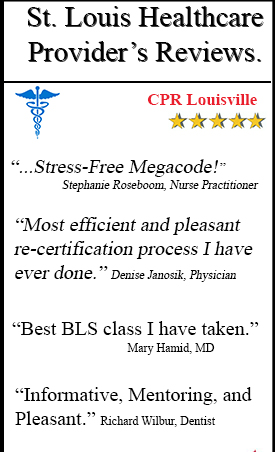
Given the high-risk, high-reward nature of this technique, the role of training and certification cannot be overstated. Healthcare providers are obligated to seek and maintain current ACLS and BLS training to ensure they possess the necessary skills to manage advanced airways effectively. Training programs emphasizing a hands-on approach to airway and resuscitation techniques are invaluable, providing the practical experience needed to perform flawlessly under pressure. A learning environment that reduces stress during training scenarios is particularly beneficial, as it allows providers to internalize the complex sequence of actions, boosting their confidence during a genuine emergency. Continuing education is the professional requirement for all providers to master and flawlessly execute the AHA guidelines.
The successful management of a patient in cardiac arrest is largely defined by the ability of the clinical team to adapt their CPR technique once an advanced airway is secured. This fundamental shift mandates continuous chest compressions at 100 to 120 per minute, paired with asynchronous ventilations at a rate of one breath every six seconds. This approach is the cornerstone of effective ACLS airway management, maximizing perfusion and minimizing harmful pauses. Applying these life-saving techniques correctly requires a commitment to rigorous, regular training and certification. By understanding and mastering this critical difference in technique, medical professionals are empowered to perform at the highest level, making the most profound difference possible in the life of a patient.
FAQs
What changes when performing chest compressions with an advanced airway in place?
When an advanced airway (such as an endotracheal tube or supraglottic airway) is secured, rescuers no longer need to pause compressions for ventilations. Instead of the traditional 30:2 compression-to-ventilation ratio, chest compressions should be performed continuously at a rate of 100-120 compressions per minute. Ventilations are given separately at a rate of one breath every 6 seconds (10 breaths per minute) without interrupting compressions. This approach maximizes perfusion and improves outcomes during cardiac arrest.
How should ventilation be delivered once an advanced airway is inserted?
Once an advanced airway is in place, ventilation should be administered at a rate of one breath every 6 seconds, which equals 10 breaths per minute. Each breath should be delivered over 1 second with enough volume to produce a visible chest rise. It’s crucial to avoid hyperventilation, as excessive breathing can increase intrathoracic pressure, decrease venous return to the heart, and reduce the effectiveness of CPR.
Do rescuers still need to switch positions during CPR with an advanced airway?
Yes, rescuer fatigue remains a concern even with an advanced airway in place. Compressors should still switch every 2 minutes (or about every 5 compression cycles) to maintain high-quality compressions. The transition should happen quickly—ideally in less than 5 seconds—to minimize interruptions. Since compressions are now continuous, the person providing ventilations can continue their role without switching positions.
Why is continuous CPR possible with an advanced airway?
An advanced airway provides a secure, isolated route for ventilation that protects the airway from aspiration and allows for effective oxygenation without interrupting chest compressions. Unlike basic airway management techniques (such as bag-mask ventilation), advanced airways remain in a fixed position and don’t require repositioning between compressions. This eliminates the need to stop compressions for breaths, allowing for uninterrupted blood flow to vital organs and improving the chances of successful resuscitation.
Call to Action
Ready to master advanced CPR techniques and life-saving skills? CPR Louisville offers comprehensive CPR certification in Louisville and BLS classes in Louisville designed to prepare you for real-world emergencies. Our American Heart Association training site provides stress-free, hands-on instruction in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid. Whether you need initial certification or renewal, our expert instructors ensure you gain the confidence and competence to respond effectively. Enroll in the best CPR classes in Louisville today and become prepared to save lives!